Pancreatic Cancer Action
Saving lives through early diagnosis
We are the only UK charity that specifically focuses on improving pancreatic cancer survival rates through early diagnosis in everything we do.

Concerned
We’re here to help. Find out about pancreatic cancer, its symptoms, risks and other useful information.
Read more
Diagnosed
Receiving a diagnosis can be worrying. We can guide you through the disease, its treatments and the next steps.
Read more
Pancreatic cancer
In the UK, almost 10,500 people are newly diagnosed with pancreatic cancer each year. Find out all you need to know about pancreatic cancer.
Read moreKey facts about pancreatic cancer
Pancreatic cancer is the UK’s 5th biggest cancer killer.
29 people are newly diagnosed with the disease every day.
Pancreatic cancer receives just 3% of research funding.
Take action
Help us improve the survival rates of pancreatic cancer by taking action in honour of a loved one, as a personal challenge or by simply supporting the cause.
Latest news
Here you can explore the latest news on pancreatic cancer, the charity, and our supporters.
The content you will find here includes updates, and insights that help raise awareness and support our mission in the fight against pancreatic cancer.
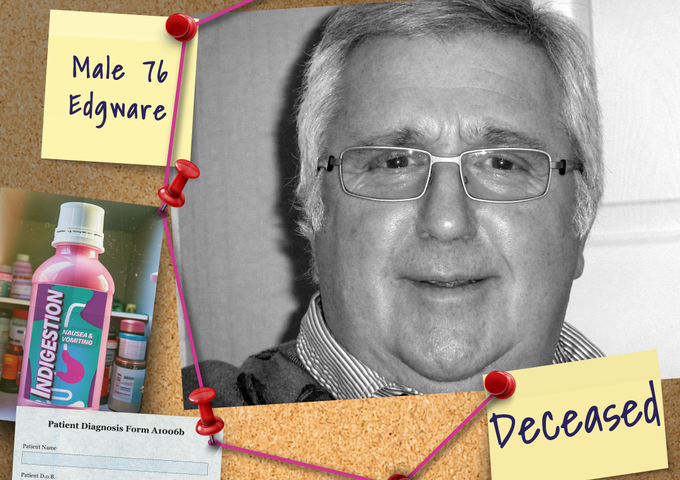
Edgware man falls victim to deadly killer
There is a deadly killer at large in the UK, claiming 26 lives every single day. For Denise Gradus, it took her father, Tony Fox, just one year after his diagnosis. Now she’s sharing his story to help others spot the signs early and stop this killer in it
Read more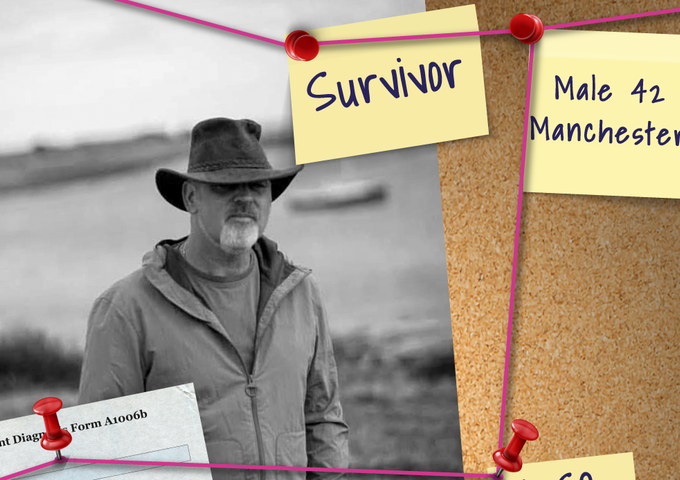
Manchester man spared by deadly killer
There is a deadly killer at large in the UK, claiming 26 lives every single day. For Martin Graham, that killer came for him at just 42 years old but he refused to give in.
Read more
Pancreatic cancer surgeon warns of symptoms you should never ignore
A leading pancreatic cancer surgeon has urged the public not to overlook early warning signs that could indicate one of the UK’s deadliest diseases.
Read more






