Pancreatic cancer is a silent killer and other myths
- Posted: 10 April 2018
- 3 min read
Being diagnosed with cancer can be a stressful time for patients, friends and families. The statistics surrounding pancreatic cancer in particular can understandably cause anxiety, and internet searches can often lead to misinformation that can cause further worry. Here we have compiled a short list of the common myths surrounding pancreatic cancer that will hopefully answer some of the questions you might have.
Pancreatic cancer is a silent killer.
This is a common misconception which is fuelled by lack of awareness of the signs and symptoms of the disease.
There are signs and symptoms of pancreatic cancer, which may seem vague and sometimes cross over with other illnesses. It can be easy to brush of indigestion, mid-back pain and weight loss, but knowing that they are symptoms of pancreatic cancer can save lives.
Our advice is if you experience one or more of these symptoms which are persistent and not normal for you – visit your GP.
By increasing awareness of the signs and symptoms of pancreatic cancer, more referrals for scans and potentially life saving surgery can be issued to patients.
Pancreatic cancer is always deadly.
Pancreatic cancer can be treated – with surgery – if diagnosed early enough. In other words, if there is no sign that the tumour has spread beyond the pancreas and you are fit enough to undergo surgery, your doctors may decide to remove the tumour.
Although pancreatic cancer is the UK’s fifth biggest cancer killer and the survival rate is just 5%, it is important to remember that there are lots of survival stories from a variety of different people. Early diagnosis is possible.
Read some of our survivor stories

Graham's story
Graham describes how he went from being a fit and healthy man living with IBS, to being diagnosed with pancreatic cancer and undergoing life changing surgery.
Read more
Lizz's story
Lizz was diagnosed with pancreatic cancer years after experiencing initial symptoms, including bloating and unusual smelling urine. Now thankfully in recovery, she has turned her attention to raising funds and awareness for pancreatic cancer.
Read more
Briony's story
Briony was diagnosed with pancreatic cancer when she was just 26 years old after she had been experiencing symptoms for as long as 5 years before.
Read moreThere is only one kind of pancreatic cancer
Pancreatic cancer occurs when a malignant tumour forms in the pancreas. There are two main types of pancreatic cancer:
-
Exocrine tumours make up most of all pancreatic cancers.
The most common type of exocrine tumour is called pancreatic ductal adenocarcinoma (PDAC) and comes from cells that line the ducts in pancreas that carry digestive juices into the intestine. There are other rarer kinds of exocrine tumours of the pancreas including Aden squamous carcinomas and undifferentiated carcinomas.
-
Neuroendocrine tumours (NETs) can be either benign (non-cancerous) or malignant (cancerous) and develop in the hormone-producing cells of the neuroendocrine system, which is spread throughout the body. NETs can appear in different organs, including the pancreas.
Pancreatic neuroendocrine tumours (pNETs) form in the pancreas' hormone-producing cells. These are less common than other pancreatic tumours and are classified as either functional (hormone-producing) or non-functional (non-hormone-producing). Functional tumours are usually detected earlier due to symptoms caused by hormone overproduction. Non-functional tumours don’t produce hormones but are more likely to be cancerous.
Most NETs occur randomly, but some people have a genetic condition, such as Multiple Endocrine Neoplasia Type 1, that increases their risk.
Types of pNETs include:
- Insulinoma: Produces too much insulin, causing symptoms like low blood sugar, frequent urination, and headaches.
- Gastrinoma: Produces gastrin, leading to stomach ulcers, cramps, and greasy stools.
- Somatostatinoma: Affects digestion and blood sugar control, causing diarrhoea, weight loss, and diabetes symptoms.
- VIPoma: Causes loose stools, dehydration, and fatigue.
- Glucagonoma: Raises blood sugar, leading to diabetes symptoms, skin rashes, and mouth sores.
Functional tumours cause symptoms due to hormone overproduction, while non-functional tumours are more likely to be cancerous but may not show symptoms until later.
Pancreatic cancer only affects men
Pancreatic cancer affects men and women equally. Everybody has a pancreas, its main functions being to help break down food; and use and store energy from food. It is found deep inside the body, behind the stomach and in front of the spine.
The estimated lifetime risk of contracting pancreatic cancer is relatively low at 1 in 73 for men and 1 in 74 for women.
Pancreatic cancer only affects older people
The likelihood of having pancreatic cancer does increase with age, this is the biggest risk factor. The average age of diagnosis of pancreatic cancer is 72. However, there is evidence that shows people of all ages can be diagnosed with pancreatic cancer.
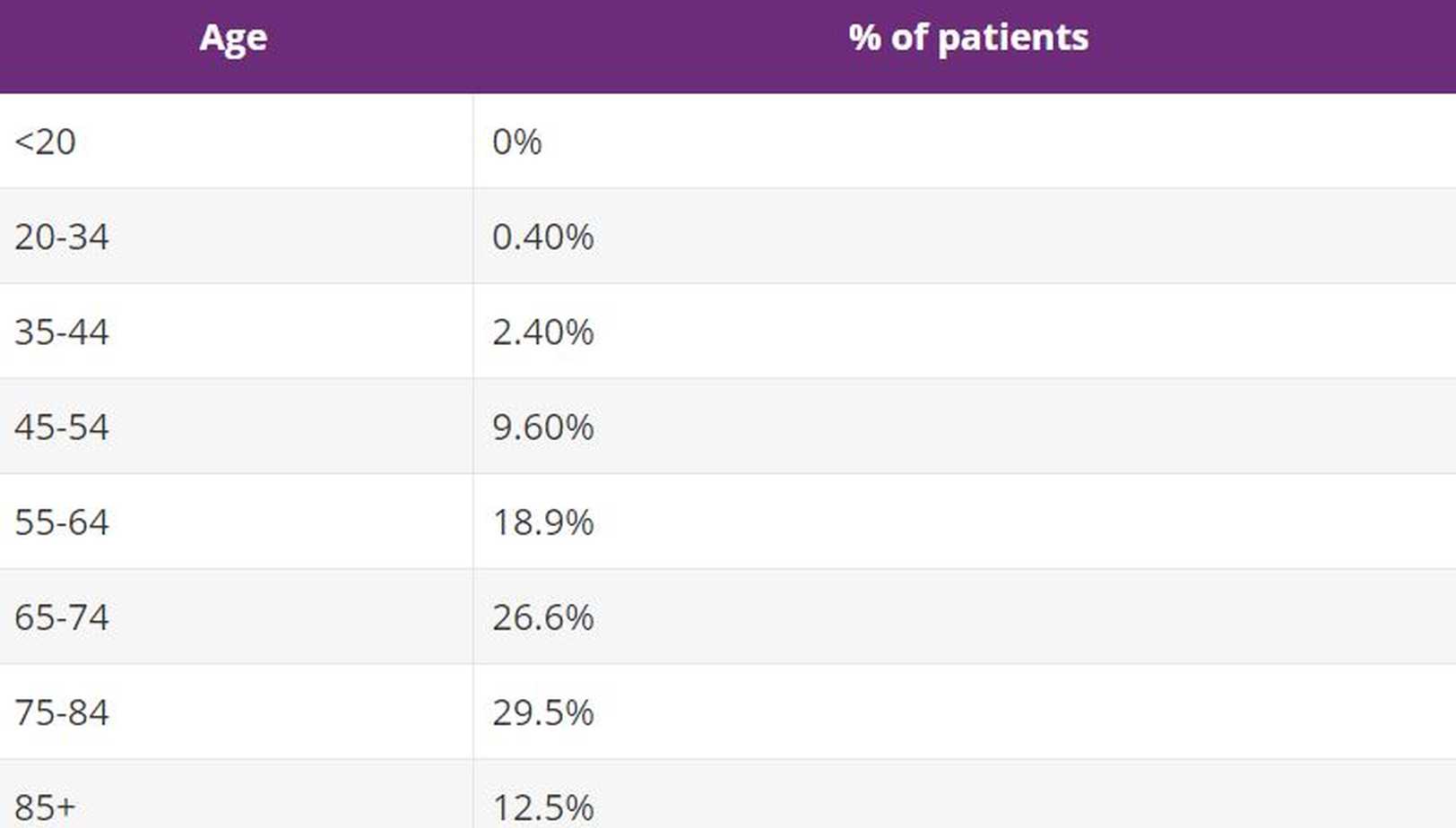
40% of all patients diagnosed in England between 2005 and 2009 were under the age of 69. This table shows percentage of pancreatic cancer cases associated with each bracket in the UK.
Clinical trials are for people who have run out of options
If a clinical trial is available to take part in, they are always optional. They offer the opportunity to trial new treatment, which may or may not be more successful than previous treatments for a particular disease. Clinical trials help doctors and researchers learn how best to treat diseases in the future and provide important evidence for future research projects.
There are three (clinical) stages a drug (or other treatments) passes through before it becomes available as an accepted treatment. Before a drug can be assessed in a trial there will have been many years of development in research laboratories, the initial results of which suggest that there is a potential theoretical benefit to using the drug in patients.
If you are ever worried that you might experiencing signs or symptoms of pancreatic cancer, it is important that you express your concerns to your GP.