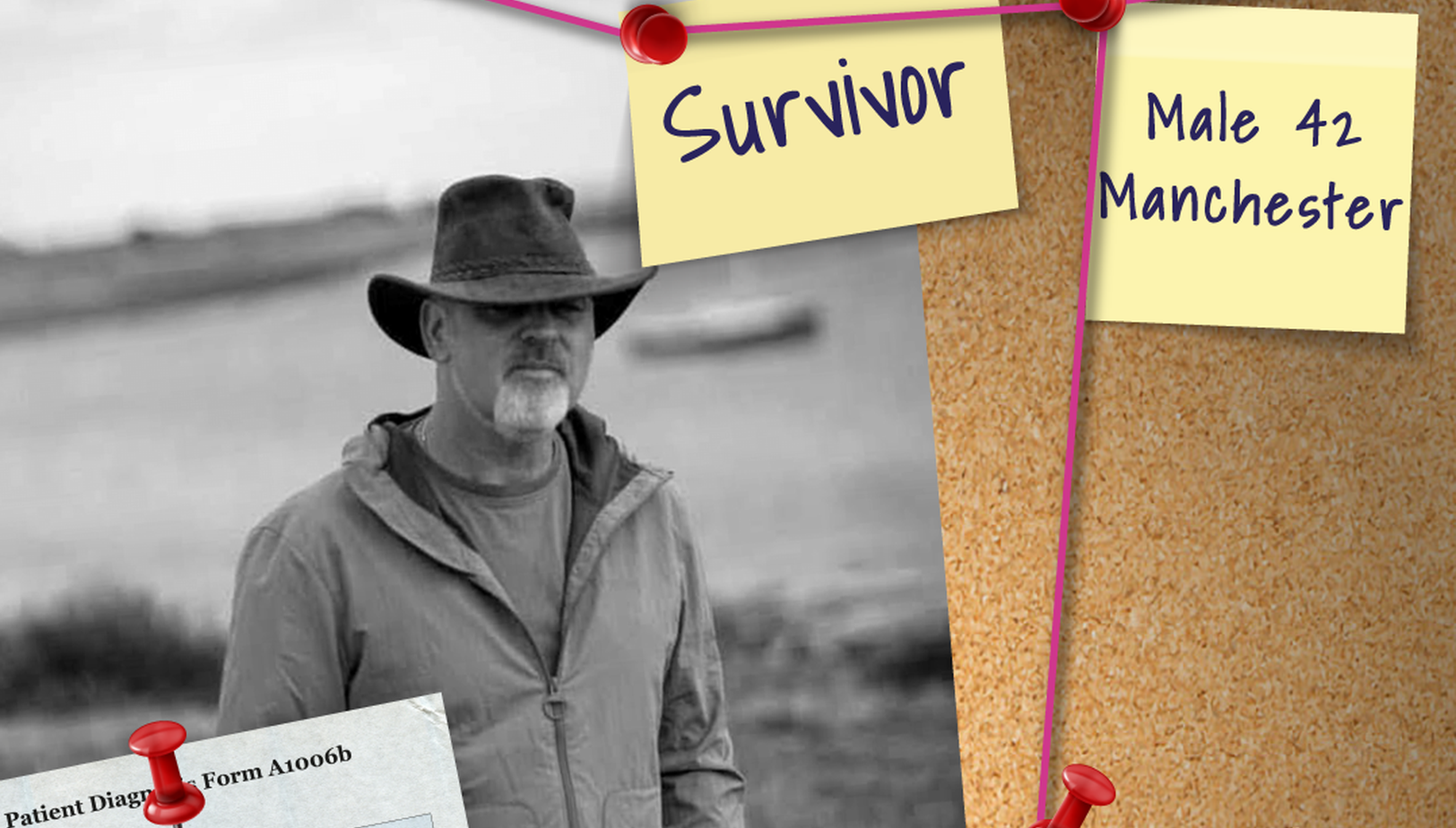
Martin Graham's Story
- Posted: 31 October 2025
- 6 min read
“My name is Martin Graham, and when I was 42 years old, I was diagnosed with pancreatic cancer.
Martin Graham
The symptoms started in early 2014 with bowel changes, blood in the toilet, and pain in my upper back. I think the first symptom was the blood in the toilet. I also had severe night sweats. I would wake up saturated and need to change the sheets.
I went to see the GP after a few weeks of it not settling down, and I was sent to have a colonoscopy. It was performed in a mobile unit in a car park. I’ll never forget speaking to the doctor in that mobile unit when I went back for my results, him telling me that I didn’t have cancer, but a form of ulcerative colitis. I had proctitis: inflammation of the lining of the rectum. I was then referred to the local hospital’s gastroenterologist, who started me on treatment.
I was expecting to start feeling better. I was told I was in ‘remission’ from the proctitis, and yet I still had all my symptoms. The back pain was the worst symptom. It was terrible. Worse after eating, worse when lying down, a horrible gnawing pain.
I kept going back to the GP. I had blood tests, but they all came back normal. They tried giving me PPIs to treat reflux. I remember saying to one GP, “I cannot take these for six weeks and then come back to you. I think I’ll be dead.”
In late October, we ordered a rare Chinese takeaway for our son’s birthday treat. We had that on the Friday. I’m not sure if that meal brought things to a head, but that night I got out of bed with pain so severe I collapsed to the floor. By Monday, during a work meeting, my boss told me I was turning yellow before his eyes.
I went straight to A&E. My wife met me there, as she works at the hospital. My bloods were taken, and we waited for the results. Some hours later, a young doctor came to speak to us. He explained my liver function test was extremely abnormal. He suggested it was most likely gallstones, but considering how deranged the results were, he opted to admit me with a view to having an ultrasound scan the following day.
The scan was performed the following day. Alarm bells should have rung, because they wheeled me straight from the ultrasound into an MRI scan, ahead of anyone else who was waiting. The following morning, the ward doctor came to speak to me. My wife had just left after a quick visit before starting her shift. He told me the scans showed a 5 cm mass at the head of my pancreas. I had to call my wife back to speak to her. We were both in shock.
The doctor didn’t even consider it could be something other than a cancerous tumour. We asked if it could be benign, but were told it wasn’t likely. We had considered pancreatic cancer because of the vague symptoms, but I was young and fit. It didn’t make sense. I’d just been climbing Kinder Scout a few days earlier, and cycling 40 plus miles the weekend before.
We had four children at home, ranging from 15 to 27 years old. My wife had to tell them I had this terrible cancer, then tell our parents and siblings. It was just such a horrendous shock for everyone.
Before I was allowed home, I was sent for a CT scan to stage the cancer, and we were quickly passed over to the most remarkable HPB doctor, who, although fairly young, had had her own experience of cancer. She understood firsthand what we were trying to get our heads around. She explained the upcoming process: my case would be discussed at the MDT meeting, and the team would come up with a plan.
We had faith. We were in a great area for healthcare. Salford Royal made the quick diagnosis and would go to MDT with surgeons from Manchester Royal Infirmary and oncologists from The Christie cancer hospital. We went back to the hospital a week later to find out what the plan of action would be. We were told the tumour was inoperable. It was wrapped around my portal vein. Fortunately it hadn’t spread further.
I was booked in for a test called ERCP, to take biopsies, get images, and insert a stent. I was so hopeful after having this, as the doctor performing it seemed surprised by what he saw. He said it didn’t look like what he was expecting. I remember telling my wife, but also saying, “I don’t want you to get your hopes up.” Then my HPB doctor came to see me before I was allowed home, and she also said there was hope. Her words were: “I hope you’re my one in a million.”
The biopsies were sent away, and we went home, praying and hoping for a miracle. We were due back in clinic a week later, after another MDT. Unfortunately, the biopsies came back as adenocarcinoma, and the MDT agreed it was too risky to operate. I could only be offered palliative chemotherapy. My tumour was considered locally advanced.
At no point did we ask, how long, or what percentage. We just didn’t want to know. We tried to take back some control. We ate only whole organic food, mainly fish, chicken, eggs, vegetables, and fruit. I drank only green tea or lemon in hot water. I walked every day. I even got my bike out for short rides. It was really important to me to feel like I was doing something, to take some control back. Even sitting outdoors instead of being cooped up inside helped.
There was a slight delay fitting my central line, as I developed a nasty flu like virus. I started my first round of chemotherapy, FOLFIRINOX, in mid-December. I’d go into The Christie for the day, get hooked up to the drip, have a short bolus, and then leave with a pump. It was a cocktail of chemo. My regime was every other Friday, and a nurse would come out on Sunday to remove the pump. I was told it could make me very sick.
The first few weeks were hard going, I’d sleep more than I was awake. Before my 4th chemo, my bloods were taken as usual two days prior, but my neutrophils were too low and they deferred my treatment. I think that was my lowest point.
I continued on with my super healthy diet, and my bloods recovered amazingly. We researched ways to support my immune system and rebuild my bloods during chemotherapy. Fortunately, they never went low again. We carried on every other week until 12 weeks were done, and it was time for an interim scan. Another positive was my tumour marker (CA19-9), which was reducing each fortnight.
One day, not long after the scan, we’d gone out for a short cycle and came home to a letter, an appointment to meet a surgeon at Manchester Royal Infirmary. We couldn’t quite comprehend what this meant, but we dared to be hopeful.
We met the most amazing surgeon, the man who saved my life. He was optimistic and said, “Now we have a chance of a complete cure. It is possible.” Whipple surgery was booked for 17th April 2015.
The surgery took almost 11 hours. When my surgeon opened me up, he could see the tumour was still wrapped around my portal vein. I guess he had two choices: sew me back up or attempt to carry on. Thank God he continued. He resected my portal vein.
I went straight to ICU afterwards. The Whipple is a huge operation, and I went home 10 days later, feeble and frail, with very little energy or appetite. I started slowly, walking to one lamppost, then the next day, a little further. Slowly, slowly, I built myself back up.
By August, I was back up Kinder Scout. By September, I was back at work. All scans since then, touch wood, have been clear.
If I could change one thing about the diagnosis of pancreatic cancer, it would be this: please have hope. Never give up. When you say “pancreatic cancer” to people, they assume there is only one outcome. But I, and many more besides me, am living proof there most definitely is hope.
Since my recovery, I’ve taken on the Three Peaks Challenge to raise funds for pancreatic cancer research, and completed two 50 km ultra challenges for other important causes. I’m proud to be able to give back, to show that life can go on, and thrive, after diagnosis.”
Deadly killer
Pancreatic cancer is the deadliest common cancer. Spotting the signs could save your life. Do you know the symptoms?
Take a look at our campaign that exposes the truth: pancreatic cancer is a silent killer that doesn’t wait or discriminate. Recognising the symptoms early and acting fast could save your life, or someone else’s. When you know the signs, you have a chance to fight back against this deadly killer.
Learn more