Subscribe to our email newsletter
Be kept in the loop about our latest news on pancreatic cancer, the charity and our supporters.
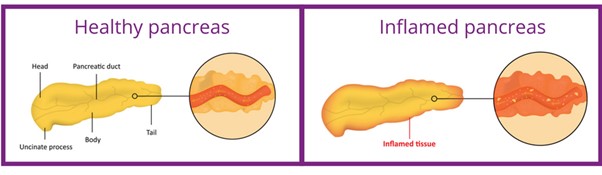
Pancreatitis is an inflammation (swelling and soreness) of the pancreas. There are two main types: acute pancreatitis and chronic pancreatitis.
| Acute | Chronic |
|---|---|
| Sudden, severe pain in centre of tummy | Frequent episodes of tymmy pain |
| Tummy swelling | Recurring Indigestion |
| Nausea/vomiting | Recurring nausea & vomiting |
| Diarrhoea | Weight loss |
| Indigestion | Jaundice |
| High Temperature- above 37.5 °C | Loss of appetite |
| Jaundice- yellowing of eyes & skin | Needing to urinate often* |
| Fatigue* | |
| Being thirsty* |
* symptoms of new onset diabetes
 The information provided in this site, or through links to other websites, is not a substitute for medical or professional care and should not be relied upon as such. Read our disclaimer.
The information provided in this site, or through links to other websites, is not a substitute for medical or professional care and should not be relied upon as such. Read our disclaimer.
Sources and references for this information product will be supplied on request. Please contact us quoting the Information Product number below:
| Information Product № | Published | 08/09/2022 | |
|---|---|---|---|
| Last Updated | 26/09/2022 | Next Review Due | 26/09/2025 |