I have Type 3c Diabetes – what is that all about?
 This week is #NationalDiabetesWeek and social media has been full of interesting facts and hints and tips on how to manage either Type 1 or Type 2 diabetes. What I have noticed though is that no-one has, thus far, mentioned Type 3 diabetes. This hasn’t come as a surprise.
This week is #NationalDiabetesWeek and social media has been full of interesting facts and hints and tips on how to manage either Type 1 or Type 2 diabetes. What I have noticed though is that no-one has, thus far, mentioned Type 3 diabetes. This hasn’t come as a surprise.
A year before I was diagnosed with operable pancreatic cancer, I was told that I may have Type 2 diabetes. However, I wasn’t overweight, nor did I have a family history of the disease. We now know that it was probably the cancer causing the blood sugar level elevations and this link between new-onset diabetes without weight gain (which can occur 1-3 years before a pancreatic cancer diagnosis) is something that we at Pancreatic Cancer Action are investigating in our research programmes.
 For all of these years (nearly 9) I have believed that I have Type 2 diabetes. However, at a recent consultation with my new Diabetologist, I discovered that I have in fact got Type 3c Diabetes.
For all of these years (nearly 9) I have believed that I have Type 2 diabetes. However, at a recent consultation with my new Diabetologist, I discovered that I have in fact got Type 3c Diabetes.
This I had never heard of before and so went about trying to find out more. I looked at some informed websites including Diabetes UK and found nothing. Not even a mention. And not all of the medical profession has heard of this type of diabetes either – unless they are specialists in this field.
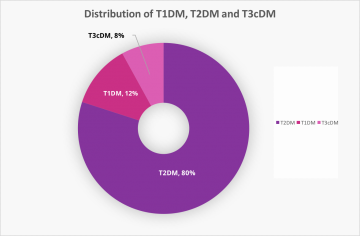
Never being one to give up, I kept on researching. I have since found out that, of all diabetes cases Type 3c makes up about 8% ((From Cui Y & Andersen DK 2011 Pancreatogenic diabetes: special considerations for management. Pancreatology 11 279–294. Copyright 2011 S Karger AG. Data from Hardt et al. (2008).)) – not a lot, but not insignificant either.
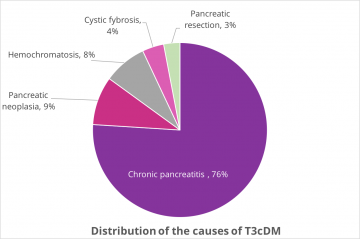 Type 3c Diabetes is usually characterised by the fact that the patient has had all or part of their pancreas resected due to cancer or cystic lesions or other diseases of the pancreas such as pancreatitis and cystic fybrosis. ((From Cui Y & Andersen DK 2011 Pancreatogenic diabetes: special considerations for management. Pancreatology 11 279–294. Copyright 2011 S Karger AG. Data from Hardt et al. (2008).))
Type 3c Diabetes is usually characterised by the fact that the patient has had all or part of their pancreas resected due to cancer or cystic lesions or other diseases of the pancreas such as pancreatitis and cystic fybrosis. ((From Cui Y & Andersen DK 2011 Pancreatogenic diabetes: special considerations for management. Pancreatology 11 279–294. Copyright 2011 S Karger AG. Data from Hardt et al. (2008).))
Patients often have Pancreatic Exocrine Insufficiency (malabsorption) and are on Pancreatic Enzyme Therapy (PERT) to help them get their nutrients from food.
Initially, my diabetes was considered a ‘side-show’ to the pancreatic cancer and rightly so. Treatment for it started with a combination of gliclazide medication and diet, but over the years my glucose control has declined. Gradually an insulin regime was introduced and, with increasing lack of glucose control (despite being very strict with my diet) the gliclazide has been removed, metformin added (slow release) daily, with insulin injections with meals and snacks and at bedtime.
My diabetes is difficult to manage – I am strict with my carb intake (to the point of being obsessive) and I have taken advantage of new technology in the form of a Freestyle Libre monitor system to help me regularly check my glucose levels without the need to prick my fingers. This is at great expense to me as this system is not funded by the NHS, and each monitor (which lasts 2 weeks) costs about £50.
What is difficult for me is that there is little or no information for patients on how to manage Type 3c diabetes. Do we follow a regime for Type 2 patients or Type 1? Not knowing makes me feel like all of this is a bit of trial and error. I’m lucky to be very closely monitored by my specialists who are helpful in finding strategies I can adopt to get my sugar levels under better control.
I am also lucky that, following my pancreatic cancer diagnosis nearly 9 years ago, my primary health concern is now my diabetes control. And, while it is a nuisance and an intrusion into every-day living, this is something I can live with because I am living many years after being diagnosed with pancreatic cancer – something that happens for only the very few.
Founder and Chief Executive
Pancreatic Cancer Action
June 15th 2016