Chemotherapy device delivers more effectively to tumours and reduces side effects
Researchers in the USA have devised a method of delivering the chemotherapy combination, FOLFIRINOX directly to pancreatic cancer tumours which not only halted tumour growth but in some cases shrank the tumour while reducing the toxic effects of the chemotherapy on other parts of the body.
In pancreatic cancer the effectiveness of chemotherapy can be reduced because pancreatic tumours have a dense stroma and lots of fibrous connective tissue surrounding them which act as a barrier to the delivery of the drugs directly to the tumour.
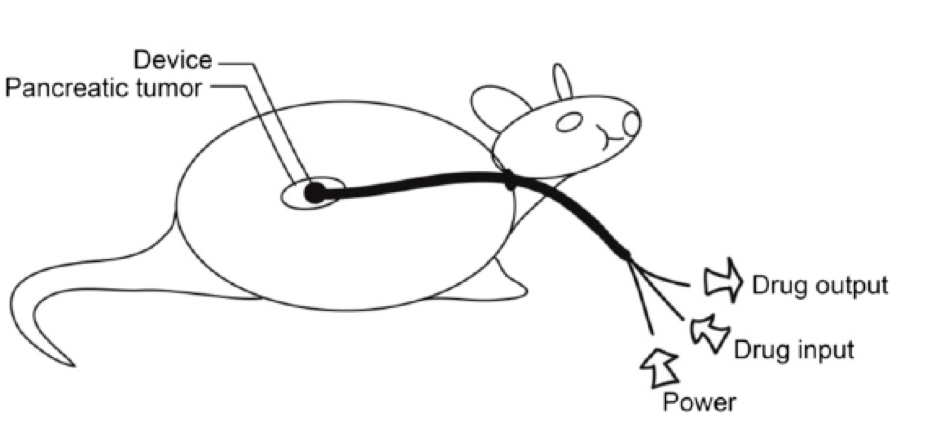
Using mouse models, the scientists devised an “iontophoretic” device to deliver the chemotherapy through the abdomen directly to the tumour through the use of an electric field.
Published in the journal, Proceedings of the National Academy of Sciences ((Byrne et al., (2016) Iontophoretic device delivery for the localised treatment of pancreatic ductal adenocarcinoma. PNAS doi:10.1073/pnas.1600421113)) the researchers found that mice treated for seven weeks with FOLFORINOX via the device had significantly greater tumour response (shrinkage or lack of growth) than mice treated in the standard way through an IV line. This response, the authors suggested, was because a much higher concentration of the chemotherapy drugs reached the tumour with the device than via an IV line .
As well as more effective delivery, the impact on other parts of the body was significantly reduced making the treatment more tolerable.
FOLFIRINOX is a first-line treatment for pancreatic cancer and has been shown to halt or shrink tumors in many patients. However, because it is so toxic to the rest of the body, there are many who cannot tolerate it when it is delivered through the bloodstream, therefore it is not a therapy that can be used in most patients.
Surgery to remove the pancreatic tumour is currently the best chance of cure, but unfortunately only 10% of patients are eligible for surgery.
The hope is that the new device will halt and potentially shrink tumours so that more patients with localised and locally advanced pancreatic cancer will eventually qualify for surgery. This could potentially improve the longer-term survival of pancreatic cancer patients.
The scientists are hoping to get the device into clinical trials in humans in the next few years.