Subscribe to our email newsletter
Be kept in the loop about our latest news on pancreatic cancer, the charity and our supporters.
Pancreatic cancer is the fifth biggest cancer killer in the UK and is expected to rise. As survival improves in other cancers, pancreatic cancer receives just 3% of research funding and has no routine screening test.
The disease is diagnosed too late for surgery in approximately 80-90% of cases and even with surgical intervention, recurrence is common. One-year survival rate is around 20% and five year is under 8%, a figure that has not significantly improved in around forty years.
The disease affects men and women equally with little variation in these figures.
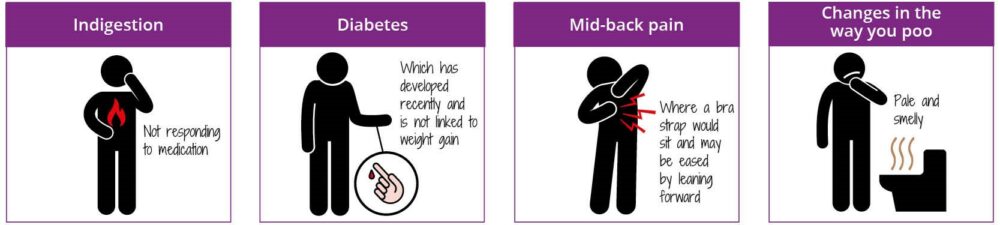
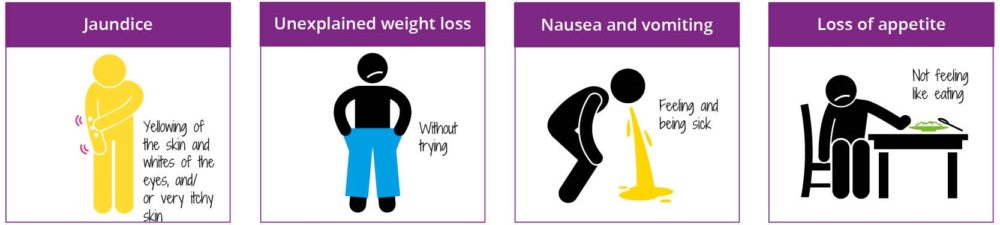
Primary care plays an important role in the early diagnosis of all cancers. Being aware of your high-risk patient groups and the symptoms of the disease leads to earlier referral, less appointments before diagnosis and can save lives.
NICE guidelines state that patients with any abdominal symptoms or diabetes and weight loss should be referred for a CT (or ultrasound if CT unavailable) within 2 weeks.
Any patient aged 40 and over with jaundice should also be referred on the two weeks wait pathway.
Any patient with a diagnosis of new onset diabetes, over the age of 60 with a BMI of less than 30 should be referred for a CT scan.
Currently, almost half of pancreatic cancer cases are diagnosed as an emergency presentation. These cases are far more likely to be late-stage presentations. Knowing the risk, signs and symptoms associated with pancreatic cancer is vital to increase GP referral and early diagnosis.
NG17 – Type 1 diabetes: diagnosis & management. Last updated August 2022.
NG85 – Pancreatic Cancer in Adults: diagnosis and management.
 The information provided in this site, or through links to other websites, is not a substitute for medical or professional care and should not be relied upon as such. Read our disclaimer.
The information provided in this site, or through links to other websites, is not a substitute for medical or professional care and should not be relied upon as such. Read our disclaimer.
Sources and references for this information product will be supplied on request. Please contact us quoting the Information Product number below:
| Information Product № | Published | 21/02/2024 | |
|---|---|---|---|
| Last Updated | 04/03/2024 | Next Review Due | 04/03/2027 |